What is Septum Deviation?
Septum deviation commonly referred to as “septoplasty“. Nasal congestion, an all too familiar complaint within our community, affects a significant part of adults, with chronic nasal congestion plaguing approximately one third of the population. The reason behind this issue lies within the nasal septum, the central partition that dutifully separates our nostrils.
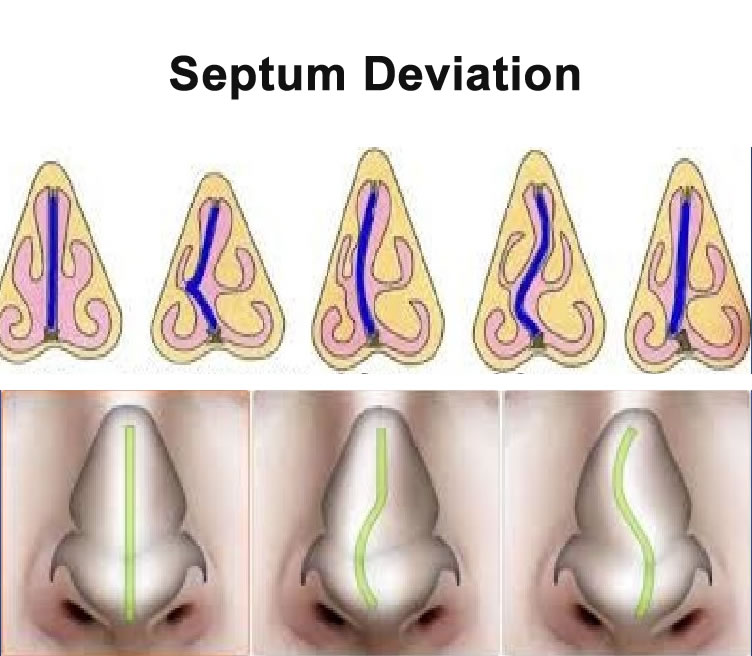
This septum, composed of cartilage at its anterior and a delicate bony structure at its posterior, is adorned with a protective mucous membrane. However, it’s worth noting that deviations from the midline, aptly named septum deviations, are prevalent among nearly 80% of adults, yet most of them do not reach a threshold that prompts any notable grievances.
What is the difference between Rhinoplasty and Septoplasty
what causes the formation of such deviations?
The primary instigator behind this phenomenon is nasal trauma. These traumas can originate from incidents occurring during gestation or during and after birth. Additionally, various traumas experienced in childhood, whether minor or major, can incite alterations in the growth points of the nasal septum.
Such disturbances lead to increased cartilage production, which, in turn, causes the septum cartilage and/or bone to contort as growth persists. In some cases, fractures may even manifest within the septum cartilage. The severity, shape, and direction of these deviations hinge upon the magnitude and orientation of the trauma, often leading to undesirable changes in the external appearance of the nose.
Let’s examine the significance of the complaints that have arisen:
- Nasal congestion, mouth breathing, and snoring: Generally, a fixed obstruction materializes on the side afflicted with deviation, while the opposing side experiences intermittent congestion due to occasional swelling of the nasal concha. Unbeknownst to many, individuals with deviations tend to find relief by lying on the side of their deviation, as it facilitates smoother airflow. Interestingly, even if the degree of deviation remains constant, the sensation of congestion and discomfort intensifies after the age of 30. Sleeping with an open mouth can leave one waking up with a parched and sticky throat, especially during the morning hours. Consequently, sleep quality is compromised, leaving individuals feeling unrested. Moreover, the difficulty in breathing through the nose slightly diminishes overall exertion capacity.
- Frequent upper respiratory tract infections: Notably, individuals with significant deviations tend to experience a higher frequency of upper respiratory tract infections, often requiring an extended recovery period.
- Recurrent nosebleeds: Those afflicted with pronounced deviations may suffer from sporadic nosebleeds, attributed to the thinning and drying of the mucosa within the protruding area.
- Impaired sense of smell: Deviations can impede the passage of odor molecules, obstructing their arrival at the olfactory region located in the upper part of the nose. This, in turn, leads to difficulties in discerning scents.
- Facial pain: In some cases, contact between the deviated septum and the nasal mucosa can give rise to facial pain, often manifesting as a dull ache in the anterior region of the face. While not particularly severe, it remains an irksome discomfort.
- Postnasal drip: Another consequence of septum deviations is the occurrence of postnasal drip, wherein excess mucus trickles down the back of the throat, causing irritation and discomfort.
It is important to note that while deviations do not directly induce heart or lung disease, they can exacerbate pre-existing conditions, thereby exacerbating symptoms. Understanding the impact of septum deviations on overall well-being allows individuals to seek appropriate care and interventions to mitigate the associated challenges.
How is the diagnosis made?
Diagnosing a nasal septum deviation involves a thorough examination of the nasal passages. By gently widening the nostrils using a specialized instrument known as a nasal speculum, the anterior portion of the septum is inspected. To gain a comprehensive view of the posterior part of the septum, nasal concha, and the openings of the sinus canals into the nose, an endoscopic examination is performed.
This entails the use of a nasal endoscope, a slender instrument equipped with a tiny camera and light at its tip, which allows for an intranasal exploration.
These examination methods are painless and swift, enabling a prompt assessment. In certain cases, when additional nasal issues such as excessive growth of the nasal concha, sinusitis, or polyps are present, sinus tomography may be conducted to thoroughly evaluate the nose and surrounding sinus structures.
How is the treatment done?
Septoplasty can be carried out under general anesthesia.Before the operation, an assessment is conducted by the anesthesiologist to evaluate any potential obstacles or risks, along with performing relevant tests.
At What Ages and Seasons Is Septoplasty Surgery Performed?
The timing for septoplasty surgery typically occurs after the age of 16-17 for girls and 17-18 for boys when cartilage-bone development is largely complete. There is no upper age limit for the procedure unless specific contraindications exist.
In exceptional cases, septoplasty may be performed in children, especially when complete obstruction of nasal breathing, sleep apnea, or adverse effects on the development of the mouth, jaw, and teeth are present.
Termed “child septoplasty,” this procedure involves limited intervention and correction without disturbing the growth points of the nasal septum, considering that children are still undergoing growth and development. In approximately half of these cases, reoperation may be necessary at the age of 17-18. Septoplasty can be performed at any time of the year, without any specific seasonal limitations.
In summary, accurate diagnosis of septum deviation involves careful examination of the nasal passages, while treatment primarily revolves around septoplasty, a surgical procedure that addresses the deviation. The age at which the surgery is performed depends on the completion of cartilage-bone development, with no upper age limit, and in certain cases, children may undergo septoplasty with cautious considerations.
How is Septoplasty Surgery Performed?
Septoplasty surgery is performed through an incision made inside the nose, allowing access to the nasal septum. The procedure involves addressing the excessive curvature of the bone and cartilage, aiming to correct the deviation. The curved bone is carefully broken and removed, while the cartilage deviations can be corrected by removing the excess and repositioning it within the nose whenever possible. Dissolvable stitches are then used to seal the wound. However, in cases where there is significant deviation outside the nose, high deviation, or deviations at the tip of the septum cartilage, the surgical approach may require an open technique, which involves removing the skin of the nose.
The duration of the surgery varies depending on the type of deviation and the chosen surgical approach, typically ranging from 30 minutes to 1.5 hours. Following the procedure, the patient is monitored for about 3-4 hours before being discharged to go home. It is important to note that correcting crooked noses with deviations that form a C-shape or S-shape, where the nose is deviated to the right or left from the midline, solely through the nasal septum can be challenging. In such cases, successful outcomes necessitate correcting both the external appearance and the internal structure of the nose. This involves performing a combined aesthetic and functional nose surgery known as “septorhinoplasty.”
In summary, septoplasty surgery involves accessing the nasal septum through an incision within the nose. The excessive bone and cartilage curvatures are addressed and corrected, with the option of an open technique for complex deviations. The duration of the surgery depends on the specific case, and post-operative observation precedes the patient’s discharge. It is essential to consider a comprehensive approach, such as septorhinoplasty, for optimal results in cases where both functional and aesthetic aspects of the nose need to be addressed.
Postoperative
Following septoplasty surgery, patients may experience mild pain, which can be effectively managed with painkillers. It is important to note that septoplasty does not cause any changes in the shape of the nose, nor does it typically result in swelling or bruising. After the surgery, soft silicone pads known as doyle splints are placed inside the nose. These pads have a tubular center, allowing for nasal breathing as long as it is not obstructed by dried mucus or blood clots.
If only septoplasty is performed, the tampons are usually removed after 2-3 days. However, if concha surgery or rhinoplasty is performed in conjunction with septoplasty, the tampons are removed after 5-7 days. The removal process is quick and painless, taking only 10-15 seconds. In some cases, dissolvable sutures may be used to stitch the nasal mucosa and septum together, allowing for an unbuffered surgery.
It is common to experience some bleeding or leakage from the nose for 1-2 days after the operation, followed by discharges mixed with mucus in the subsequent days. Crusting in the nose can occur and last for 1-2 weeks. These crusts can be gently cleaned by using physiological saline to soften them. Rest is generally recommended for 7-10 days following surgery. However, if the patient’s work does not involve strenuous activity and there are no complications after the operation, it may be possible to resume work and travel as early as the 5th day. After 10 days, normal water can be drawn into the nose and lightly blown.
It is important for patients to follow postoperative instructions provided by their surgeon and attend any necessary follow-up appointments for proper healing and recovery.
What Complications Can Be Seen After Septoplasty Surgery?
While complications following septoplasty surgery are rare, it is important to be aware of potential risks. These complications may include:
- Bleeding: Some bleeding is expected after surgery, but excessive or prolonged bleeding may require medical attention.
- Septal Hematoma: This refers to the accumulation of blood between the nasal cartilage and the lining. It is a rare complication that may require drainage to prevent complications.
- Infection: Although uncommon, there is a risk of developing an infection at the surgical site. Prompt medical attention is necessary if infection is suspected.
- Septum Perforation: This complication involves a full-thickness hole in the nasal septum. It can occur as a result of mucosal tears during nasal surgeries. Wide tears in septoplasty surgery should be sutured separately to minimize the risk of perforation.
- Adhesion in the nose: Adhesions, also known as synechiae, are abnormal scar tissue formations that can occur in the nasal cavity. They may cause nasal obstruction and may require additional treatment to address.
- Recurrence of Deviation: In some cases, the nasal septum may partially or fully deviate again after surgery, leading to recurrent symptoms. This can occur due to various factors, including the natural healing process or incomplete correction during surgery.
- Collapse on the back of the nose: Removing excessive septum cartilage can weaken the nasal support, potentially resulting in a condition known as “saddle nose” or nasal collapse. To prevent this, a sufficient amount of solid cartilage should be preserved during the surgery.
